Root canal treatment, also known as endodontic therapy, is a crucial dental procedure that saves a tooth which has become infected or severely damaged. Far from the fearful reputation it once held, modern root canal therapy is a highly effective and generally comfortable process designed to alleviate pain and preserve your natural tooth, preventing the need for extraction. Understanding why a root canal is necessary, what the procedure entails, and how to navigate the recovery period is key to a smooth experience and successful long-term outcome. This guide offers a comprehensive overview to demystify root canals, empowering you with knowledge for better oral health.
Read Also: Oral Hygiene Tips: Brushing, Flossing & More Explained
Why a Root Canal is Needed: Recognizing the Signs of Infection
A root canal becomes necessary when the soft inner part of your tooth, known as the pulp, becomes infected or inflamed. The tooth pulp contains nerves, blood vessels, and connective tissue, extending from the crown of the tooth down to the tip of the roots. When this pulp is compromised, it can lead to significant pain and, if left untreated, the infection can spread, potentially causing an abscess, bone loss, and even systemic health issues.
The most common causes of pulp infection or damage include deep tooth decay that has penetrated to the pulp, repeated dental procedures on the same tooth, cracks or chips in the tooth that expose the pulp, or even a traumatic injury to the tooth.
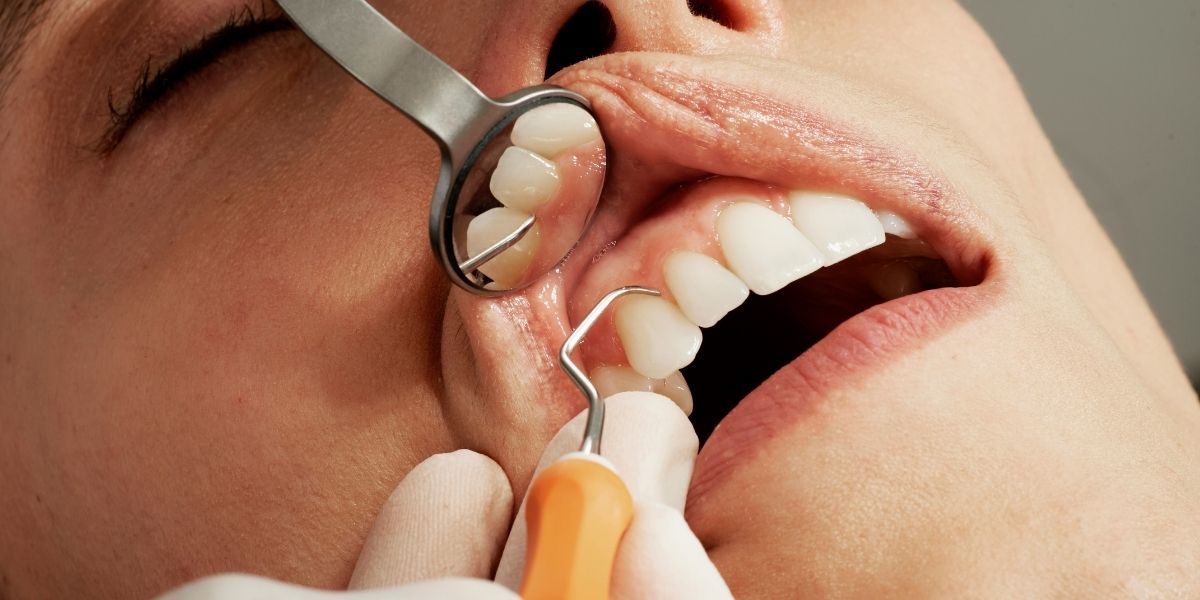
Photo Credit: Unsplash.com
Recognizing the signs and symptoms that indicate a need for a root canal is crucial for timely intervention. These often include:
Persistent Tooth Pain: This pain can range from mild sensitivity to a severe, throbbing ache that doesn’t subside. It may spread to your jaw, face, or other teeth.
Sensitivity to Hot and Cold: Lingering sensitivity to temperature, especially after the hot or cold source is removed, can be a clear indicator of pulp damage.
Tenderness to Touch and Chewing: If your tooth hurts when you bite down or apply pressure, it suggests inflammation around the root.
Swollen, Tender Gums: Swelling, tenderness, or a recurring “pimple” or boil on the gums near the affected tooth can signal an underlying infection (abscess).
Tooth Discoloration: A darkening or grayish discoloration of the tooth can occur if the pulp has died.
Ignoring these symptoms or delaying treatment can lead to the infection spreading, increased pain, and ultimately, the loss of the tooth. A root canal saves the natural tooth, which is always the best option for maintaining chewing function, natural appearance, and preventing adjacent teeth from shifting.
The Root Canal Procedure: Step-by-Step
Modern root canal therapy is typically performed by a general dentist or, for more complex cases, by an endodontist (a dental specialist in root canals). The procedure, often completed in one or two appointments, is designed to be as comfortable as possible.
The process begins with diagnosis and anesthesia. The dentist will conduct a thorough examination, including X-rays, to confirm the extent of the infection and determine if a root canal is the appropriate treatment. Before starting, local anesthesia is administered to completely numb the affected tooth and surrounding gum tissue, ensuring a pain-free experience during the procedure. Many patients report that the discomfort during a root canal is no more than that of a standard filling.
Next, a dental dam is placed. A small, thin sheet of rubber is isolated around the tooth being treated. This keeps the tooth dry, clean, and free from saliva and bacteria throughout the procedure, which is vital for preventing re-infection.
Then, the dentist creates a small access opening in the crown of the tooth to reach the infected pulp chamber and root canals. Using tiny, specialized dental instruments called files, the infected and inflamed pulp tissue, along with any bacteria and debris, is carefully removed from inside the tooth’s crown and root canals. This meticulous cleaning and shaping process ensures all infected material is eliminated and the canals are prepared for filling. An antiseptic solution is also used to thoroughly disinfect the canals.
Once the canals are thoroughly cleaned and shaped, they are filled and sealed. The empty space within the root canals is filled with a biocompatible, rubber-like material called gutta-percha. This material is inserted along with an adhesive sealer to completely fill and seal the canals, preventing future bacterial contamination.
Finally, the tooth receives a temporary or permanent restoration. A temporary filling is placed over the access opening in the crown of the tooth to protect it until a permanent restoration can be placed. In most cases, especially for back teeth that endure significant biting forces, a dental crown is recommended as the final step. The crown protects the treated tooth from fracture, restores its full function, and allows it to blend seamlessly with your natural smile. This final restoration appointment typically occurs a few weeks after the initial root canal, giving the tooth time to heal.
Root Canal Recovery: What to Expect and How to Heal Smoothly
After a root canal procedure, it is normal to experience some mild discomfort and sensitivity as your body begins the healing process. Understanding what to expect and following your dentist’s post-procedure instructions are crucial for a smooth and swift recovery.

Photo Credit: Unsplash.com
In the immediate aftermath (first 24-48 hours), your mouth will likely remain numb for several hours due to the local anesthesia. It is important to avoid eating or drinking anything until the numbness completely wears off to prevent accidental biting of your cheek or tongue. Some tenderness around the treated tooth and mild soreness in your jaw from keeping your mouth open during the procedure are common. Over-the-counter pain relievers such as ibuprofen or acetaminophen are usually sufficient to manage any discomfort. Your dentist may prescribe stronger medication if needed, or antibiotics if the infection had spread significantly. Applying a cold compress to the outside of your cheek can help reduce any swelling, though significant swelling is not typical. Rest is important during this initial period.
For the next few days to a week, it is essential to be mindful of your diet and oral hygiene. Stick to soft foods that require minimal chewing, such as soups, yogurt, mashed potatoes, smoothies, and soft pasta. Avoid chewing on the treated tooth, especially if a temporary filling is in place, as hard, crunchy, or sticky foods could dislodge it or damage the tooth. Also, avoid extremely hot or cold foods and beverages, as sensitivity may persist. Maintain gentle oral hygiene by carefully brushing and flossing around the treated area. Rinsing with warm salt water several times a day can help keep the area clean and promote healing. Avoid harsh mouthwashes for a few days. It is common to feel a slightly different sensation from the treated tooth compared to your other teeth for some time. However, contact your dentist immediately if you experience severe pain or pressure that worsens or lasts for more than a week, visible swelling inside or outside your mouth, an allergic reaction to medication, a bad taste in your mouth (which could indicate a spreading infection), or if your temporary filling or crown comes out.
Read Also: Conquering Canker Sores: Prevention, Relief, and Healing Strategies
The long-term care of your treated tooth is paramount for its success. A permanent crown or filling is crucial to protect the tooth from future fracture and restore its full function. Your dentist will typically schedule a follow-up appointment to place this permanent restoration once the tooth has healed. Continue to maintain excellent daily oral hygiene practices, including brushing twice a day and flossing once daily, and attend regular dental check-ups and cleanings. A properly treated and restored tooth can last a lifetime, functioning just like your other natural teeth. While a root canal saves the tooth, consistent care ensures it remains a healthy and functional part of your smile for many years to come.







